Isaac Allan Judd arrived on Saturday November 3 at 3:01 AM. Here’s the story of his arrival.
The start of labor
Our midwife Kim stopped by at 9:30am to see how I was doing, and to discuss if we wanted to take any herbal measures to try to move labor along. As it turned out, my contractions picked up pretty soon after she left, and were about 3 minutes apart just before noon, marking the start of official “active” labor. We called Kim back and made a plan for her to come to the house again after dinner, when we figured I’d be fairly well dilated or least ready for a check-in. During the day I generally paced and leaned on the counter, couch or wall when a surge happened, with Brian helping me breathe through the harder contractions. I also spent some time in the hot tub to relax. The afternoon passed uneventfully, with regular contractions, as I sought to stay hydrated and relaxed, if not distracted. My water broke at 6:45pm and the three midwives all arrived at our house by 7:30pm.
The tub
I had spent a lot of time on my feet since Thursday night, and because I enjoyed being in the hot tub off my feet so much, I took Kim up on her offer to bring a birthing tub (despite the fact that every previous time a birthing tub was mentioned, I said I was not interested). So, between 8 and 9pm on Friday night, Brian was called into action to figure out how to get tens of gallons of 98 degree water into a large inflatable tub that the midwives set up in the nursery. I understand it involved removing the shower head and plumbing a connection of the garden hose. (Of course if you’ve never tried to get a coiled garden hose into your shower, Brian doesn’t recommend it. There is a reason they are for outdoor use!)

You sure this will work?
I was oblivious to this late night plumbing, other than wondering why the midwives and Brian kept leaving me to labor alone (there are 3 of them, how is it none of them is in here with me?) and then being so touched that when the tub was ready they had laid out towels in the hallway for me to walk on, which I assumed were to keep me from dripping a mess on the floor (but in reality were due to the inevitable drips and leaks of the hose and bailing water back and forth from the bathroom to the tub!). It felt really good to be in the tub, and I stayed in there for maybe 20 – 30 minutes until I was fully dilated, then got out a while to push – first on all fours, then on the birthing stool – then got back in again when my right leg started feeling weak and I wanted to get my weight off my feet again.
A slight complication
I should mention at this point that my abdomen shape had changed between Thursday and Friday, with the appearance of two separate sections and a “band” across the middle (as though there was a belt around my waist). Even when I was fully dilated my contractions were a bit irregular and my pushing wasn’t making much progress. The midwives were concerned that my uterus wasn’t working well as a single muscle which would definitely be a problem. So, one of the times they left me in the tub was so they could caucus. They asked me to stop pushing and recommended that we transfer to the hospital to get a medical diagnosis on the “banding”. At 11:30pm they got me out of the tub, dried off and dressed, Brian packed a bag for me, and we got in the car to go to Emerson Hospital. Brian drove me and managed to not only drive safely, but to also coach me to keep breathing and not push during the 20 minute drive, while Kim followed us in her car, so she would continue to be with us as a doula. She had called ahead so they were expecting me at the hospital, and took me straight into labor and delivery, bypassing the emergency room.
It turned out that as the baby had descended, somehow my bladder had gotten above my uterus to form the “top” segment above the “band” (which was the space between my uterus and bladder), and the nurses drained over 2L of urine with a catheter. We were surprised because I had spent a lot of time in the bathroom at home, but evidently was passing other fluids and not peeing as often as I had assumed. It did explain why I had such a feeling of relief, almost euphoria, when my water broke. It had released the pressure built up between my bladder and uterus, which felt great! But after that, all the water I’d drunk had probably stayed with me for hours, building up pressure and causing my contractions to push against my bladder rather than helping the baby to make progress descending.
Back to pushing
Once the bladder issue was resolved, the doctor on duty said everything else looked great and invited me to continue pushing. I pushed with increasing intensity for the next couple hours. We got a bar set up on the bed so I could try squatting, rather than being on my back. Due to what turned out to be a strained groin, I ended up doing most of my pushing on my side, with one leg in a stirrup and the other being held by a nurse or Kim or Brian, as I closed my eyes and pushed. I was usually able to get 2-3 breaths worth of pushing in for each contraction. Everyone was so supportive in updating me on my progress, praising my pushing, encouraging me to relax between contractions, and holding a hand or leg or bringing me water to drink or a cloth for my face. Kim encouraged me to reach down and feel the baby’s head, which was reassuring and motivating for me to continue pushing.
The doctor would pop in every so often (I have no idea how often – every 15 – 20 minutes?) to check on me. He said he wanted to respect my wishes for avoiding intervention, but that he was growing increasingly concerned about the baby’s health given the long duration of labor and pushing, and the fact that its heart rate would dip down into the 90s or even 80s when I pushed. I understand that he was quite patient for an Ob/Gyn, even though I felt like I was on the clock to get this baby out before his patience ended! In order to help with my energy and to help keep baby’s oxygen levels up they gave me an oxygen mask. I highly recommend pure oxygen if you’re feeling tired. For the next 2 hours I felt stronger than I had the previous few hours.
I got the baby’s head to crown about 3 inches but just didn’t have much more pushing in me after a couple hours at home plus almost three hours in the hospital. If I knew it would be a few more pushes or 5 more minutes, I think I could have definitely continued, but Kim and the nurses couldn’t say – afterwards, Kim thought it might be 30-45 more minutes, and I surely didn’t have that much more pushing in me. So, we decided to get a little help from the vacuum extraction to get the baby delivered more quickly.
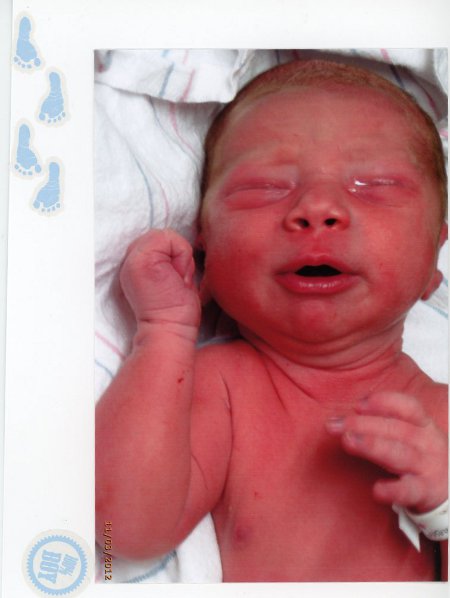
Isaac is born!
After two pushes, the head was out, and with one more push, his shoulders and body were out too! The baby immediately gave a loud cry, and the doctor was clearly relieved to see such a healthy pink yelling baby, the nurse interjected , “It’s a boy,” and the doctor announced “he’s FINE!” as he rolled his chair back. They laid my baby on my belly and we got to meet one another. I can’t describe the elation of delivery. Yes there was the “ring of fire” and yes it was intense. But I was so focused, with eyes closed, the only thing in the world at that moment was concentrating on delivery of the baby. And then, to feel that release and hear the cry, was just amazing. I said hello and cooed at him and cried with happiness and relief.
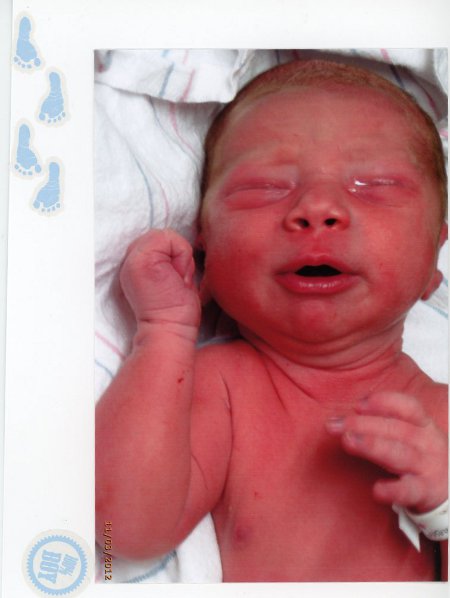
Isaac Allan Judd
Recovery
We recovered in the hospital on Saturday, which was really nice. They took care of me, helped me to the bathroom, and offered lots of helpful advice. The Sheldons stopped by to meet Isaac (and bring Brian a clean shirt – he had packed a bag for me but brought nothing for himself!) before they left for a trip. Another friend came to visit and helped us with breastfeeding to make sure Isaac was latching properly. The nurses kept an eye on my bladder, to make sure it was recovered and operating properly before I went home. Isaac was thriving from the start – he even flipped himself over on the examining table right after he was born! – nursed well and passed all of his tests. We were able to get discharged Sunday evening so we could come home and rest in our own bed, without the 2x per night exams and lights, etc. I stayed in bed for 5 days on Kim’s advice, glad that Brian and several friends who stopped in could take care of me while I recuperated and took care of Isaac.
Reflecting
Overall, we are so happy with the experience and the support. It really was just as we hoped – we labored at home as long as possible, were ready to give birth there if everything had gone well, but were able to get medical care when we needed it. In our mind, this is not a “failed” home birth, it was a complete success. I got so many comments about my preparation, mental attitude, strength and resilience, and how well Brian and I were able to work and communicate together. I took no drugs and avoided a C section, so we were very happy with the result. I did have some tearing between the hard pushing – much harder than the midwife would have recommended, but I was on a deadline to avoid the C-section! – and the forced extraction at the end. So that takes a while longer to recover, but in the scheme of things is a really small part of the overall experience.
If someone told me 5 years ago I’d have 4 days of prelabor contractions, 15 hours of active labor including 3+ hours of pushing, all the things a body goes through, not get more than 3 hours of sleep at a stretch for weeks, and think these were easily some of the happiest days of my life, I would have thought they were crazy. But on November 7 we were watching the snow fall outside, enjoying a favorite meal Brian prepared, with him wearing our son in a wrap so we could sit down to have our first dinner as a 3-person family, and I thought my heart might just burst.


Write a comment